Tuberculosis (TB) is a serious infectious disease that primarily affects the lungs, and understanding your TB test results is crucial for your health.
Millions of people around the world are screened for TB every year, yet many are unsure what a positive TB test really means. A positive result doesn’t always indicate active illness it can also signify latent TB infection, where the bacteria are present but inactive.
TB testing is most commonly done through the tuberculin skin test (TST), also known as the Mantoux test, or through blood tests like the interferon-gamma release assay (IGRA).
Each method has its own way of showing a positive result, whether it’s a visible bump on the skin or a laboratory report indicating infection.
Knowing what a positive TB test looks like, and how it’s interpreted, is essential for taking the right next steps and ensuring proper medical care.
What is a TB Test?
A TB test is a medical procedure used to determine if someone has been infected with the bacteria that cause tuberculosis, Mycobacterium tuberculosis. TB can remain dormant in the body for years, which is why testing is important even when no symptoms are present. There are two main types of TB tests: the tuberculin skin test (TST) and the TB blood test, also called an interferon-gamma release assay (IGRA).
The tuberculin skin test (Mantoux test) involves injecting a small amount of purified protein derivative (PPD) just under the skin of the forearm. After 48 to 72 hours, a healthcare professional checks the injection site for induration, a raised, firm area. The size of the induration, measured in millimeters, helps determine if the test is positive based on a person’s risk factors. Redness alone is not considered a positive result.
The TB blood test (IGRA) measures the immune system’s response to TB bacteria by detecting specific proteins released in the blood. Unlike the skin test, the IGRA does not produce a visible bump, and results are provided through a laboratory report as positive, negative, or indeterminate. Blood tests are often preferred for people who have received the BCG vaccine or cannot return for a second appointment to read a skin test.
Both tests are tools to detect latent TB infection or active TB disease. Understanding the differences between these methods is essential for interpreting results accurately and deciding on the next steps for medical care.
Understanding a Positive TB Test
A positive TB test indicates that a person’s immune system has been exposed to the tuberculosis bacteria. However, it does not automatically mean active TB disease. There are two main possibilities: latent TB infection (bacteria are present but inactive) or active TB disease (bacteria are actively multiplying and may cause symptoms). Distinguishing between the two requires further medical evaluation, such as a chest X-ray or sputum test.
For the tuberculin skin test (TST), a positive result is determined by the size of the induration at the injection site, measured in millimeters. The threshold for a positive result varies depending on individual risk factors. For example, an induration of 5 mm may be considered positive in immunocompromised individuals, while 10–15 mm may be required for healthy adults with no known TB exposure. It’s important to note that redness around the site does not indicate a positive test—only firm swelling (induration) is measured.
For the TB blood test (IGRA), results are provided as positive, negative, or indeterminate through a lab report. A positive IGRA indicates TB infection regardless of prior BCG vaccination, making it particularly useful in people who were vaccinated as children.
Factors such as age, immune system status, recent TB exposure, and prior vaccinations can influence test results. False positives and false negatives are possible, so interpretation should always be done by a healthcare professional.
What a Positive TB Skin Test Looks Like
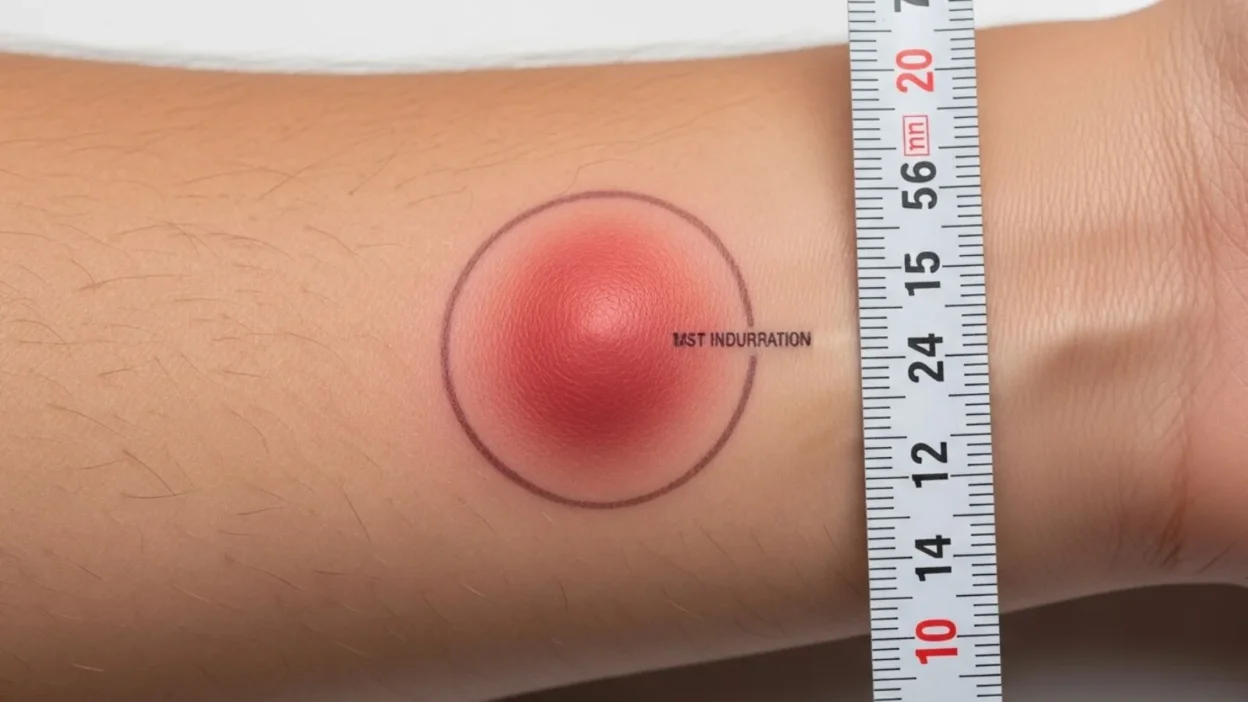
The tuberculin skin test (TST), or Mantoux test, is the most common method to screen for TB infection, and a positive result has a distinct visual appearance. After the test is administered, a small amount of purified protein derivative (PPD) is injected just under the skin, usually on the forearm. A positive reaction is not determined by redness, but by the presence of induration—a firm, raised bump at the injection site.
Healthcare professionals measure the diameter of the induration in millimeters 48 to 72 hours after the injection. The interpretation depends on a person’s risk factors: for example, an induration of 5 mm or more may be considered positive in people with weakened immune systems or recent TB exposure, while 10 mm or more is positive for individuals with moderate risk factors, and 15 mm or more for healthy adults with no known risks.
Redness around the site is common and normal, but it is not counted as part of the measurement. The bump should feel firm and raised rather than soft or flat. Some people may experience slight itching or tenderness, which is also normal.
Visually, a positive TST appears as a raised, pale to reddish bump on the skin, often oval or round. Correct measurement and interpretation by a trained healthcare professional are crucial, as mistakes can lead to false positives or negatives. Understanding this appearance helps patients know what to expect and reduces unnecessary worry about the test results.
Positive TB Blood Test (IGRA)
Unlike the tuberculin skin test, the TB blood test, also called an interferon-gamma release assay (IGRA), does not produce any visible signs on the skin. Instead, this test measures the immune system’s response to Mycobacterium tuberculosis by detecting specific proteins called interferon-gamma released by white blood cells in response to TB antigens.
A positive IGRA result indicates that a person’s immune system has encountered TB bacteria. The result is reported by a laboratory as positive, negative, or indeterminate. A positive result means the person is likely infected with TB bacteria, either as latent TB infection or active TB disease, and requires further evaluation. Unlike the skin test, prior BCG vaccination does not affect IGRA results, making it a preferred option for people who have been vaccinated or cannot return for a second appointment.
While a positive blood test confirms infection, it cannot determine whether TB is active or latent. Additional tests, such as a chest X-ray or sputum examination, are necessary to evaluate symptoms, lung involvement, and the risk of transmission.
IGRAs are highly accurate, convenient, and require only a single visit. However, factors such as immunosuppression, recent TB exposure, or laboratory errors can sometimes lead to false negatives or indeterminate results. Proper interpretation by a healthcare professional is essential to ensure the correct diagnosis and guide next steps for treatment or monitoring.
Understanding how a positive TB blood test differs from the skin test helps individuals know what to expect and emphasizes the importance of follow-up evaluation.
Interpreting Positive Results
A positive TB test signals that a person’s immune system has been exposed to Mycobacterium tuberculosis, but it does not automatically indicate active TB disease. Understanding the meaning of a positive result is crucial to taking the right next steps.
For the tuberculin skin test (TST), the size of the induration determines positivity, but this depends on individual risk factors. For example, a 5 mm bump is considered positive in people with weakened immune systems, such as those with HIV, while 10 mm or 15 mm may be required for others. In contrast, a TB blood test (IGRA) provides a lab-based result of positive, negative, or indeterminate. A positive IGRA generally indicates TB infection regardless of BCG vaccination.
A positive test could mean either latent TB infection or active TB disease. Latent TB occurs when bacteria are present but dormant; individuals usually do not show symptoms and are not contagious. Active TB occurs when bacteria multiply and cause symptoms such as persistent cough, fever, night sweats, and weight loss. Medical evaluation, including chest X-rays and possibly sputum tests, is necessary to distinguish between the two.
It is also important to recognize that false positives and false negatives can occur due to factors like previous BCG vaccination, immunosuppressive conditions, or recent TB exposure.
Next Steps After a Positive TB Test
Receiving a positive TB test result can be worrying, but it is important to understand that it does not always mean active disease. The next steps focus on confirming whether the infection is latent or active and determining appropriate treatment.
The first step after a positive test is typically a medical evaluation. Your healthcare provider may recommend a chest X-ray to check for signs of active TB in the lungs. In some cases, a sputum test or other laboratory tests may be necessary to detect bacteria directly. These follow-up tests help distinguish between latent TB infection, which is inactive, and active TB disease, which can spread to others.
For those diagnosed with latent TB infection, treatment usually involves a course of antibiotics to prevent the infection from becoming active in the future. Common regimens include isoniazid or rifampin, sometimes combined, depending on health status and risk factors. Adherence to the full course of medication is crucial to ensure effectiveness and prevent drug resistance.
If active TB disease is confirmed, treatment is more intensive, often requiring a combination of multiple antibiotics over 6 to 9 months. Patients may need to follow strict medical supervision to monitor side effects and prevent transmission.
Risk Factors That Affect TB Test Interpretation
Not all positive TB test results are interpreted the same way. Several risk factors can influence whether a test is considered positive and how it is managed. Understanding these factors is essential for accurate diagnosis and follow-up care.
One major factor is immune system status. Individuals with weakened immune systems—such as those with HIV, undergoing chemotherapy, or taking immunosuppressive medications—may have smaller reactions on a skin test, meaning even a small induration can indicate TB infection. Conversely, a healthy immune system might produce a larger reaction.
Age also plays a role. Infants and older people individuals may have atypical immune responses, making TB test interpretation more challenging. In these cases, a blood test (IGRA) is often preferred.
Previous BCG vaccination can affect the tuberculin skin test, sometimes leading to false positives. However, blood tests like IGRA are not influenced by prior vaccination, making them more reliable for vaccinated individuals.
Recent TB exposure is another critical factor. People who have been in close contact with someone who has active TB are at higher risk, and even a small induration may be considered positive.
Finally, underlying health conditions, such as malnutrition, chronic kidney disease, or diabetes, can alter immune responses, affecting both skin and blood test results.
Because these risk factors vary widely among individuals, TB test results should always be interpreted by a healthcare professional. Considering these variables ensures accurate diagnosis, appropriate follow-up testing, and timely treatment, reducing the risk of progression from latent to active TB.
FAQs About Positive TB Tests
1. Does a positive TB test mean I have TB disease?
Not necessarily. A positive test indicates infection with TB bacteria but does not automatically mean active disease. Additional tests like a chest X-ray or sputum culture are needed to determine if the TB is latent or active.
2. Can a positive TB test go away on its own?
A positive result typically remains positive for life, even after treatment for latent TB. It reflects past exposure, not necessarily current illness.
3. Why did I get a false positive?
Factors like prior BCG vaccination, exposure to non-TB mycobacteria, or incorrect test administration can sometimes cause false positives, particularly with the tuberculin skin test.
4. How soon after exposure should I test for TB?
It usually takes 2 to 8 weeks after exposure for a TB test to show positive results. Testing too early may yield a false negative.
5. Can children and immunocompromised people rely on the skin test?
Sometimes the TB blood test (IGRA) is preferred for children, the older people, or immunocompromised individuals because it is not affected by prior BCG vaccination and requires only one visit.
6. What should I do after a positive TB test?
Consult a healthcare professional promptly for further evaluation, including chest imaging and, if necessary, treatment for latent or active TB. Avoid close contact with vulnerable individuals until evaluated.
Conclusion:
A positive TB test can be alarming, but understanding what it truly indicates is essential for proper care. For the tuberculin skin test (TST), a positive result appears as a raised, firm bump (induration) at the injection site, measured in millimeters, while the TB blood test (IGRA) shows positivity through a lab report without visible signs.
Positive results indicate exposure to TB bacteria, but they do not automatically mean active disease.
Distinguishing between latent TB infection and active TB disease requires further medical evaluation, including chest X-rays and possible lab tests.
Factors such as immune status, age, prior BCG vaccination, and recent exposure can influence test interpretation, making professional guidance critical.
Prompt follow up, accurate diagnosis, and, if needed, appropriate treatment are key to preventing progression and protecting your health. Understanding the appearance and meaning of a positive TB test empowers individuals to take informed, timely action with confidence.