Cellulitis is a common bacterial skin infection that can affect anyone, but early recognition is key to preventing serious complications.
It typically occurs when bacteria, often Streptococcus or Staphylococcus, enter through cuts, scratches, or other breaks in the skin.
The first signs are usually redness, swelling, and warmth in the affected area, which can spread rapidly if left untreated.
Many people confuse cellulitis with rashes, insect bites, or allergic reactions, but its distinct appearance and symptoms make early identification possible.
In this article, we’ll guide you through what cellulitis looks like, the common symptoms to watch for, how it differs from other skin conditions, and effective treatment and prevention strategies.
By understanding these signs, you can act quickly, seek medical care, and reduce the risk of severe infections or complications. Recognizing cellulitis early is the first step to proper care.
What is Cellulitis?
Cellulitis is a bacterial infection that affects the skin and the tissues just beneath it. It usually develops when bacteria, most commonly Staphylococcus aureus, enter the body through cuts, scrapes, insect bites, surgical wounds, or other breaks in the skin. Once inside, the bacteria multiply, causing redness, swelling, warmth, and tenderness in the affected area. While cellulitis can appear anywhere on the body, it most frequently affects the lower legs, arms, and face.
People of all ages can get cellulitis, but certain groups are at higher risk. Individuals with diabetes, weakened immune systems, chronic swelling (lymphedema), or skin conditions like eczema are more prone to infection. Even minor injuries, such as a scratch or a small blister, can provide an entry point for bacteria.
Early recognition of cellulitis is crucial because the infection can spread quickly. If left untreated, it can lead to serious complications like abscess formation, blood infections (sepsis), or damage to underlying tissues. The severity of cellulitis can vary from mild redness and swelling to extensive inflammation accompanied by fever and chills.
Understanding what cellulitis is helps differentiate it from other skin issues like rashes, allergic reactions, or insect bites. By knowing the signs and risk factors, you can seek medical attention promptly and prevent the infection from worsening.
Common Symptoms of Cellulitis
Recognizing the symptoms of cellulitis early is essential for effective treatment. The infection usually begins with a small area of redness on the skin that gradually expands. This redness is often accompanied by swelling, warmth, and tenderness, making the affected area feel sore or painful to touch. In some cases, the skin may appear shiny or tight due to the swelling.
Pain and discomfort are common, and the intensity can vary depending on the severity of the infection. Some people may notice a burning or throbbing sensation in the affected area. Blisters or small pus-filled bumps may also form in more severe cases, signaling that the infection is progressing.
Systemic symptoms can accompany the local signs of cellulitis, especially if the infection spreads. These may include fever, chills, fatigue, and swollen lymph nodes near the affected area. Rapidly spreading redness or streaks extending from the infection site can indicate that the bacteria are moving through the lymphatic system, which requires immediate medical attention.
Other subtle signs may include warmth spreading beyond the red area, mild itching, or tenderness even when the skin looks normal at first. Because cellulitis can resemble other skin conditions like eczema, allergic reactions, or insect bites, paying close attention to the combination of symptoms is critical. Early recognition ensures prompt treatment, reducing the risk of complications.
What Does Cellulitis Look Like?
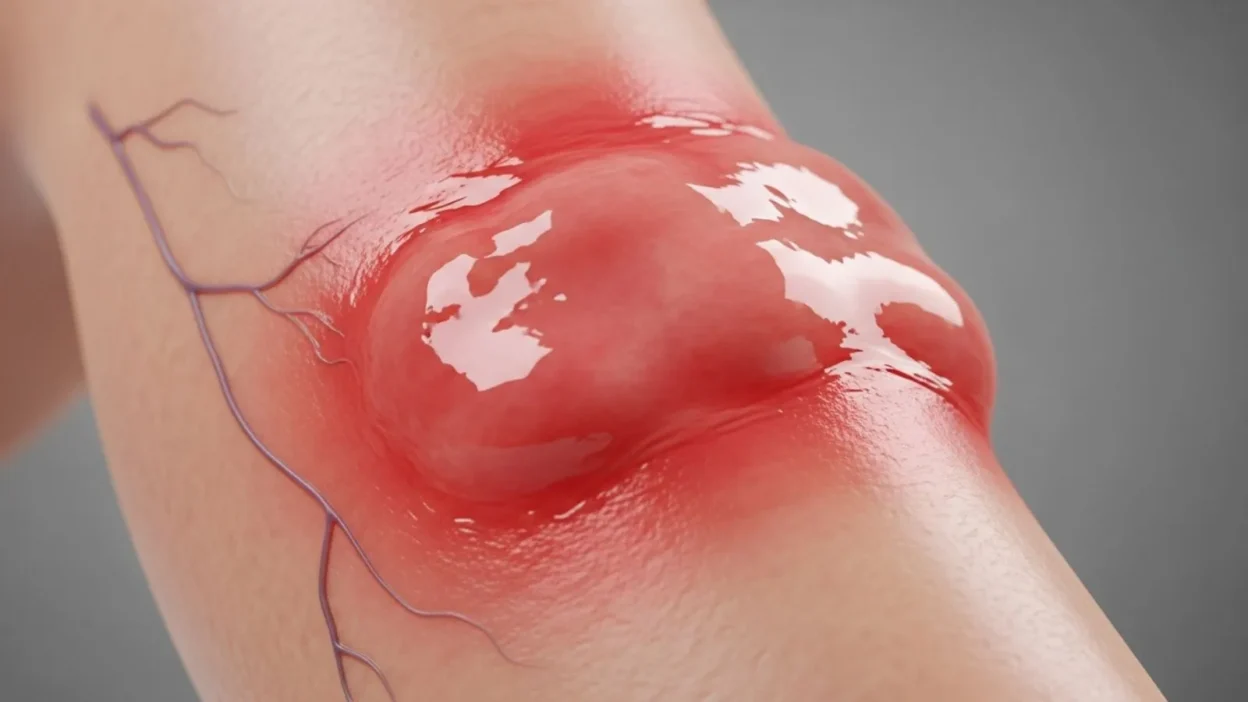
Cellulitis often presents with distinct visual signs that can help you identify the infection early. One of the most noticeable features is redness on the skin, which usually has irregular, poorly defined edges. Unlike rashes from allergies or eczema, cellulitis often spreads outward from the initial infection site, gradually covering a larger area. The affected skin may appear shiny, tight, or swollen, and pressing lightly can feel warm or hot compared to surrounding skin.
Swelling is another common sign. In many cases, the infected area feels firm or puffy, and the swelling may cause discomfort or restrict movement if it affects joints. Blisters or small pus-filled bumps can sometimes form, especially in severe cases, signaling deeper bacterial invasion. The skin may also become painful or tender to touch, with a constant throbbing or burning sensation.
Cellulitis can affect any part of the body but is most commonly seen on the lower legs, arms, and face. Red streaks extending from the infected area toward the heart can indicate that the infection is spreading through the lymphatic system, which requires urgent medical attention.
It is important to differentiate cellulitis from other skin conditions. Unlike a typical rash, cellulitis is often accompanied by swelling, warmth, tenderness, and systemic symptoms such as fever or chills. Recognizing these visual cues early is critical for seeking prompt treatment and preventing complications.
Cellulitis vs Other Skin Conditions
Cellulitis can often be mistaken for other skin conditions, making early identification challenging. Understanding the differences is essential for proper care.
Eczema, for example, usually appears as dry, itchy, and scaly patches of skin. Unlike cellulitis, eczema rarely causes warmth, pain, or rapid spreading redness. It is often bilateral (affecting both sides of the body) and may flare up over weeks rather than days.
Allergic reactions or contact dermatitis may cause redness and swelling similar to cellulitis. However, these reactions are often sudden, itchy, and accompanied by hives or small bumps, whereas cellulitis tends to be tender and warm rather than itchy. Allergic reactions typically improve when the allergen is removed or antihistamines are used.
Insect bites can also resemble cellulitis, with localized redness and swelling. However, insect bites usually have a central puncture mark and are confined to a small area. Pain is mild, and redness does not spread rapidly.
Shingles, caused by the varicella-zoster virus, appears as a painful, blistering rash following nerve pathways. It is usually unilateral and often accompanied by tingling or burning before visible signs appear.
The key distinguishing features of cellulitis are rapidly spreading redness, warmth, tenderness, and systemic symptoms like fever or chills. Red streaks extending from the infected area are a warning sign that the infection is spreading through the lymphatic system.
Correctly differentiating cellulitis from other conditions is critical. Misdiagnosis can delay treatment, increasing the risk of complications. If there is any doubt, consulting a healthcare professional is always recommended.
Causes and Risk Factors
Cellulitis occurs when bacteria enter the skin, causing infection and inflammation. The most common bacteria responsible are Streptococcus and Staphylococcus aureus. These bacteria can enter the body through even minor breaks in the skin, such as cuts, scrapes, insect bites, burns, surgical wounds, or ulcers. Once inside, the bacteria multiply, triggering redness, swelling, warmth, and tenderness in the affected area.
Certain factors increase the likelihood of developing cellulitis. People with weakened immune systems, such as those with diabetes, HIV, or undergoing chemotherapy, are more susceptible because their bodies are less capable of fighting off infections. Chronic swelling, like lymphedema, can also make the skin more vulnerable, as it stretches and becomes prone to small cracks where bacteria can enter.
Other risk factors include skin conditions like eczema, athlete’s foot, or psoriasis, which can compromise the skin barrier. Obesity, poor circulation, and previous cellulitis episodes also increase susceptibility. Additionally, cuts, puncture wounds, and surgical sites are common entry points for bacteria.
Environmental and lifestyle factors can contribute as well. For example, wet or humid environments can soften the skin, making it easier for bacteria to penetrate. Poor hygiene, walking barefoot outdoors, or frequent exposure to minor injuries can further increase risk.
Understanding the causes and risk factors of cellulitis helps in prevention and early detection. People who identify these risk factors in themselves can take extra precautions, such as proper wound care, moisturizing the skin, and monitoring for early signs of infection.
Treatment Options for Cellulitis
Cellulitis requires prompt treatment to prevent the infection from spreading and causing serious complications. The primary treatment is antibiotics, which can be administered orally for mild cases or intravenously for severe or rapidly progressing infections. Doctors typically prescribe antibiotics that target Streptococcus and Staphylococcus bacteria, and it’s important to complete the full course even if symptoms improve to prevent recurrence or resistance.
In addition to antibiotics, supportive care plays a crucial role in recovery. Elevating the affected limb can help reduce swelling, while applying warm compresses may relieve discomfort. Over-the-counter pain relievers, such as acetaminophen or ibuprofen, can help manage pain and inflammation. Staying hydrated and resting also supports the body’s immune system during healing.
For severe cases, hospitalization may be required, especially if the infection spreads rapidly, affects the face or joints, or occurs in individuals with weakened immunity. Healthcare providers may monitor vital signs, administer intravenous antibiotics, and perform blood tests to check for systemic infection.
Home care measures are also important after medical treatment. Keeping the skin clean, avoiding scratching, and monitoring the area for new redness or swelling can prevent complications. It’s essential to seek medical attention immediately if symptoms worsen or if fever, red streaks, or pus develop.
Early and proper treatment of cellulitis not only relieves discomfort but also reduces the risk of serious complications, making recognition and timely care critical.
Prevention Tips for Cellulitis
Preventing cellulitis starts with protecting the skin and minimizing the risk of bacterial infection. Since cellulitis often develops when bacteria enter through cuts, scratches, or other breaks in the skin, proper wound care is essential. Clean any minor cuts, scrapes, or insect bites promptly with soap and water, apply an antiseptic, and cover them with a clean bandage until fully healed.
Keeping the skin moisturized can also help prevent cracks and dryness that provide entry points for bacteria. People with conditions like eczema or athlete’s foot should manage these conditions carefully to maintain a healthy skin barrier. Avoid scratching or picking at skin lesions, as this increases the risk of infection.
For those at higher risk, such as individuals with diabetes, chronic swelling (lymphedema), or weakened immunity, extra precautions are necessary. Wearing protective clothing, gloves, or shoes while outdoors or performing tasks that could injure the skin helps reduce bacterial exposure. Maintaining good hygiene, including regular handwashing and bathing, also supports skin health.
Lifestyle factors play a role as well. Healthy habits, such as maintaining a balanced diet, staying active, and controlling chronic conditions like diabetes, strengthen the immune system and reduce susceptibility.
Finally, monitoring your skin daily for early signs of redness, swelling, or tenderness allows for quick action if an infection develops. Prompt treatment of even minor infections is key to preventing cellulitis from becoming serious.
By following these preventive measures, you can significantly reduce the risk of cellulitis and protect overall skin health.
When to See a Doctor
Recognizing when cellulitis requires professional medical attention is crucial, as the infection can worsen rapidly. You should see a doctor immediately if the redness or swelling spreads quickly or covers a large area. Rapid progression can indicate that the bacteria are moving through the lymphatic system, which may lead to serious complications.
Other warning signs include fever, chills, fatigue, or swollen lymph nodes near the affected area, as these systemic symptoms suggest that the infection is affecting the whole body. Pain that intensifies or pus-filled blisters forming on the skin are also signals to seek urgent care.
Red streaks extending from the infected site toward the heart are a particularly serious symptom and require immediate medical attention, as they indicate that the infection may be spreading through the bloodstream.
Even if symptoms seem mild, it’s wise to consult a healthcare provider if you have underlying health conditions, such as diabetes, immune system disorders, or chronic swelling, since cellulitis can progress more quickly in these cases. Prompt medical evaluation ensures effective treatment, reduces the risk of complications, and prevents the infection from returning.
FAQs About Cellulitis
1. Can cellulitis go away on its own?
No, cellulitis usually requires antibiotic treatment to fully resolve. Leaving it untreated can cause the infection to spread, leading to serious complications like sepsis or tissue damage.
2. How fast does cellulitis spread?
Cellulitis can spread rapidly within hours or days if untreated. Early signs include redness and swelling that gradually expand outward from the infection site. Prompt medical attention is crucial to prevent progression.
3. Can cellulitis be contagious?
Cellulitis itself is not contagious, meaning you cannot “catch” it from another person. However, the bacteria that cause it, such as Streptococcus or Staphylococcus, can spread through direct contact with open wounds, so proper hygiene is important.
4. Can cellulitis recur?
Yes, cellulitis can recur, especially in individuals with chronic swelling, weakened immunity, or previous infections. Managing risk factors and following preventive measures can reduce recurrence.
5. How long does treatment take?
Mild cases typically improve within 5–10 days of oral antibiotics, while severe infections may require 2 weeks or more of treatment, sometimes including intravenous antibiotics. Completing the full course is essential to prevent relapse.
6. Are there home remedies for cellulitis?
Home care, like elevating the affected limb, applying warm compresses, and taking pain relievers, can help relieve symptoms. However, antibiotics prescribed by a doctor are essential; home remedies alone cannot cure cellulitis.
7. How can I prevent cellulitis?
Preventive measures include keeping skin clean and moisturized, properly treating cuts and scrapes, avoiding scratching, and monitoring for early signs. People with higher risk should take extra care to protect their skin.
Conclusion:
Cellulitis is a common but potentially serious bacterial skin infection that can spread rapidly if left untreated.
Recognizing the visual signs, such as redness, swelling, warmth, and tenderness, is essential for early detection.
Paying attention to systemic symptoms like fever, chills, or red streaks extending from the affected area can help identify more severe cases that require urgent medical care.
Differentiating cellulitis from other skin conditions, such as rashes, allergic reactions, or insect bites, ensures timely and proper treatment.
Prompt medical intervention, typically with antibiotics, combined with supportive care, helps prevent complications like tissue damage or bloodstream infections.
Preventive measures, including proper wound care, moisturizing the skin, and monitoring high risk areas, can significantly reduce the risk of cellulitis.
By staying vigilant and seeking professional help when necessary, individuals can manage cellulitis effectively and protect overall skin health. Early recognition and treatment are the keys to a safe and speedy recovery.

The author behind RiddleBurst.com loves creating fun, clever, and unique riddles for all ages. Their goal is to challenge minds, bring smiles, and make learning through riddles both engaging and enjoyable.